LASER TREATMENT FOR VASCULAR LESION
The complex web of blood vessels throughout our bodies is vital in preserving our overall well-being. However, disruptions or abnormalities in these vessels can lead to vascular lesions, posing varied challenges and concerns across different age groups. Understanding these lesions, their types, and the significance of blood vessel health is pivotal for effective treatment and management.
Understanding Vascular Lesions
Vascular lesions encompass a spectrum of abnormalities affecting blood vessels, manifesting in diverse forms and presentations.
These abnormalities can emerge from various factors, spanning congenital conditions, injuries, or underlying health concerns. They often appear as visible abnormalities on the skin or within deeper tissues, presenting challenges in diagnosis and treatment.

The Importance of Blood Vessel Health
Healthy blood vessel function is fundamental for optimal blood flow, carrying vital nutrients and oxygen. Any deviation from this norm can result in issues like altered blood flow, accumulation of red blood cells, or the formation of vascular tumours or malformations. Maintaining blood vessel health is crucial for overall well-being, especially in sensitive areas like the face or hand.
Book Your Free Consultation Today Or Call (647) 560-9233
By providing your phone number you agree to receive informational text messages from laserskin.ca. Consent is not a condition of purchase. Message frequency will vary. Msg & data rates may apply. Reply HELP for help or STOP to cancel.










Types of Vascular Lesions
- Hemangiomas: These benign tumours are common in infants and can vary from superficial to deeper lesions. Some may require treatment due to rapid growth or location-based concerns.
- Venous Malformations: Abnormalities in the veins can lead to venous lakes or deeper malformations, causing issues based on size and location.
- Arteriovenous Malformations: This type involves an abnormal connection between arteries and veins, potentially leading to significant health complications if not managed properly.
- Lymphatic Malformations: Disruptions in lymphatic vessels can cause issues such as lymphatic malformations, affecting various soft tissues and presenting challenges in treatment.
- Capillary Malformations: These involve abnormal developments in the capillaries and often manifest as port-wine stains, requiring specific treatment approaches.
Treatment Options and Interventions
Effective treatment is crucial for the best results when dealing with vascular lesions. Various treatment options exist, ranging from laser therapy and surgical excision to topical applications like topical timolol.
Treatment selection relies on variables like the lesion’s type, dimensions, placement, and the individual’s age.
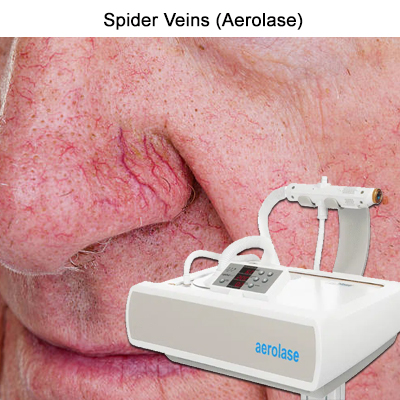
Laser treatments, such as the Aerolase laser, have shown promise in managing certain vasculatients. They offer targeted therapy, especially for smaller areas or sensitive locations. However, like any treatment, they may have associated side effects and necessitate expertise for optimal results.
A multidisciplinary team involving interventional radiologists, pediatric dermatologists, or surgeons might be essential for deeper lesions or complex cases like arteriovenous malformations. They collaborate to devise a comprehensive treatment plan tailored to the patient’s specific condition and needs.
Causes and Risk Factors of Vascular Lesions
Vascular lesions encompatientous anomalies affecting blood vessels, with causes often multifactorial. Understanding the contributing factors sheds light on their development and aids in effective management.
Genetic Influence
Genetic inclinations hold considerable sway in the development of vascular lesions. Some individuals might inherit a tendency toward specific vascular anomalies, increasing their likelihood of developing conditions like atypical vascular lesions or certain types of vascular malformations.
Pregnancy and Preterm Birth
The onset of vascular lesions in infants has been associated with pregnancy and preterm delivery. The occurrence of vascular lesions in infants has been associated with both pregnancy and premature birth. Certain lesions, such as infantile hemangiomas, often manifest within the first few weeks or months of a child’s life and might be associated with events occurring during pregnancy or birth.
Hormonal Fluctuation Children’s nasal fluctuations, especially during puberty or pregnancy, can trigger certain vascular lesions’ appearance or rapid growth. This hormonal influence is often observed in lesions like cherry angiomas or superficial hemangiomas, which might present or exacerbate during these periods.
Symptoms of Vascular Lesions
The symptoms of vascular lesions can vary widely based on their type, location, and depth within the body. They can manifest in different forms and affect various bodily systems.
Cutaneous Vascular Lesions
These lesions primarily affect the skin and can appear as vascular birthmarks, spider veins, or cherry angiomas. Their visibility often causes cosmetic concerns, although some might lead to discomfort or bleeding in certain cases.
Cerebral Vascular Lesions
Lesions affecting blood vessels in the brain might present with symptoms like seizures, headaches, or neurological deficits depending on their size, location, and involvement of critical areas in the brain.
Internal Vascular Lesions
Deeper vascular lesions within organs or soft tissues can lead to masses or irregularities felt during physical examinations. Some might remain asymptomatic, while others can cause pain, interfere with organ function, or pose health risks based on their location and size.
Diagnosis of Vascular Lesions
Accurate diagnosis of vascular lesions involves a comprehensive approach combining various examination methods to determine the nature and extent of the anomaly.
Physical Examination
Clinical assessment plays a crucial role in identifying and categorizing vascular lesions. Examination of the lesion’s characteristics, such as size, colour, texture, and location, aids in determining the type and severity of the poles.
Imaging Procedures
Sophisticated imaging techniques like MRI, CT scans, or ultrasound are instrumental in visualizing vascular anomalies and assessing their depth, size, and relationship to surrounding structures. These procedures provide valuable insights into planning treatment strategies.
Histopathological Analysis
A biopsy or histopathological analysis might be necessary in cases where the diagnosis remains unclear or to confirm suspicions. This involves examining a tissue sample under a microscope to identify specific cellular characteristics, aiding in accurate diagnosis and treatment planning.
Treatment and Management of Vascular Lesions
Medication and Drug Therapy
Treating and managing vascular lesions requires a multifaceted approach encompassing medical interventions, lifestyle adjustments, and addressing the psychological impact they might exert on individuals. Let’s delve into the diverse treatment modalities, lifestyle changes, and the psychological aspects associated with living with vascular lesions.
Surgical Interventions
Surgical interventions are often considered for larger or deeper vascular lesions that pose health risks or affect organ function. Surgical excision or procedures like embolization might be employed to address arteriovenous fistulas or complex vascular malformations.
Advances in Laser Technology
Laser therapy has significantly evolved in treating various vascular lesions. Modern laser technologies, like the Aerolase laser, offer targeted treatment for small areas or sensitive regions. These advancements provide effective results with minimal discomfort and faster recovery.
The Process of Sclerotherapy
Sclerotherapy entails injecting a solution directly into the impacted blood vessel, prompting its collapse and gradual fading. It’s commonly used for treating spider veins, venous malformations, or vascular birthmarks, offering a noninvasive approach with favourable outcomes.
Lifestyle Changes and Home Remedies
Improving Diet
While dietary alterations may not directly cure vascular lesions, a nutrient-rich diet abundant in antioxidants, vitamins, and minerals can bolster overall health. This may indirectly benefit vascular health and aid the body’s healing process.
The Role of Exercise
Regular exercise promotes blood circulation and overall cardiovascular health. While it doesn’t directly treat vascular lesions, it can contribute to maintaining optimal blood vessel function and supporting the body’s general well-being.
Tips for Pain Management
To ease symptoms for individuals enduring discomfort or pain from vascular lesions, using cold compresses or elevating the impacted area could offer relief. As advised by healthcare experts, pain management strategies can improve quality of life.
Psychological Impact of Vascular Lesions
Understanding the Impact on Self-esteem
Vascular lesions, especially when visible, can impact self-esteem and body image. Children or adults with these lesions might experience social stigma or emotional distress, highlighting the importance of addressing psychological well-being.
Strategies to Enhance Mental Health
Supportive therapies or counselling can assist individuals in coping with the emotional challenges associated with vascular lesions. Building resilience, seeking peer support, or engaging in activities that boost confidence can positively impact mental health.
Q & A
- What are the typical locations where vascular skin lesions manifest?
Vascular skin lesions can appear anywhere on the body, commonly seen on the face, limbs, or torso, and might vary based on the type of lesion and its depth within the skin.
- Are arteriovenous fistulas primarily treated through surgical intervention?
Yes, surgical intervention often serves as the primary treatment for arteriovenous fistulas, depending on the exact location and severity of the anomaly.
At what age can vascular lesions like infantile hemangiomas (IHs) typically appear?
This usually manifests within the first few weeks or months of a child’s life, often becoming noticeable in early infancy.
- How might radiation therapy be utilized in managing vascular lesions?
Radiation therapy could be considered for certain types of vascular lesions, especially those difficult to access surgically or treat through other means, aiming for the best possible result.
- Could you explain the significance of lymphatic channels in forming vascular anomalies?
A child’s lymphatic channels develop certain malformations, contributing to vascular anomalies observed in conditions like Klippel-Trenaunay syndrome.
- Are there specific risk factors associated with the development of Blue Rubber Bleb Nevus Syndrome?
While the exact reasons are not always clear, congenital factors might contribute to the development of Blue Rubber Bleb Nevus Syndrome, primarily observed in children or young adults.
- Can vascular lesions like Kaposi sarcoma affect older adults more frequently?
Yes, Kaposi sarcoma, a type of vascular tumour, tends to be more prevalent in elderly individuals but can occur in various age groups.
- How early in childhood might Sturge-Weber syndrome become apparent?
Sturge-Weber syndrome typically becomes evident in early childhood, often presenting with a port-wine stain on the face within the first year of life.
- Could you elaborate on the types of vessels involved in congenital lipomatous overgrowth?
Congenital lipomatous overgrowth primarily affects adipose tissue and blood vessels, developing soft tissue masses involving these vessels.
- Is there a particular timeframe, such as weeks or months of age, when premature infants might exhibit vascular anomalies?
Premature infants can develop vascular anomalies within weeks or months after birth, although the manifestation might vary based on individual circumstances.
Conclusion: Living with Vascular Lesions
Navigating Support Systems
Accessing support groups or seeking guidance from healthcare professionals specializing in vascular anomalies can provide valuable insights and emotional support. Engaging with communities facing similar challenges can offer comfort and practical advice.
Recent Breakthroughs and Research on Vascular Lesions
Continued research and breakthroughs in vascular anomaly studies offer hope for improved treatment modalities and better outcomes.
Remaining updated on recent advancements can empower patients and caregivers, enabling them to make well-informed choices concerning treatment alternatives.
Living with vascular lesions involves a holistic approach that goes beyond medical treatment. Incorporating lifestyle modifications, addressing psychological aspects, and staying updated on advancements in research collectively contribute to a better quality of life for individuals affected by these conditions.
